Reflux is a common condition clients see a naturopath in Perth about. Mainstream medicine usually treats the symptoms with a class of medicine called a proton pump inhibitor. The problem with these medications is that over time, they compound the problem by causing a bacterial imbalance in the gut. These medicines when used long term, lead to nutrient deficiencies as we require stomach acid to absorb certain vitamins and minerals.
Stomach acid also plays the important role of inhibiting bacteria that we swallow while consuming food and those which live in the upper respiratory tract or mouth. In fact, many cases of small intestinal dysbiosis (SIBO) are caused by oral and sinus bacteria blooming in the gut. This can cause food intolerances, excessive bloating, gas, and abdominal distension and discomfort.
Health tip: These medications should not be used as a long-term treatment approach due to the benefits being outweighed by the side effects.
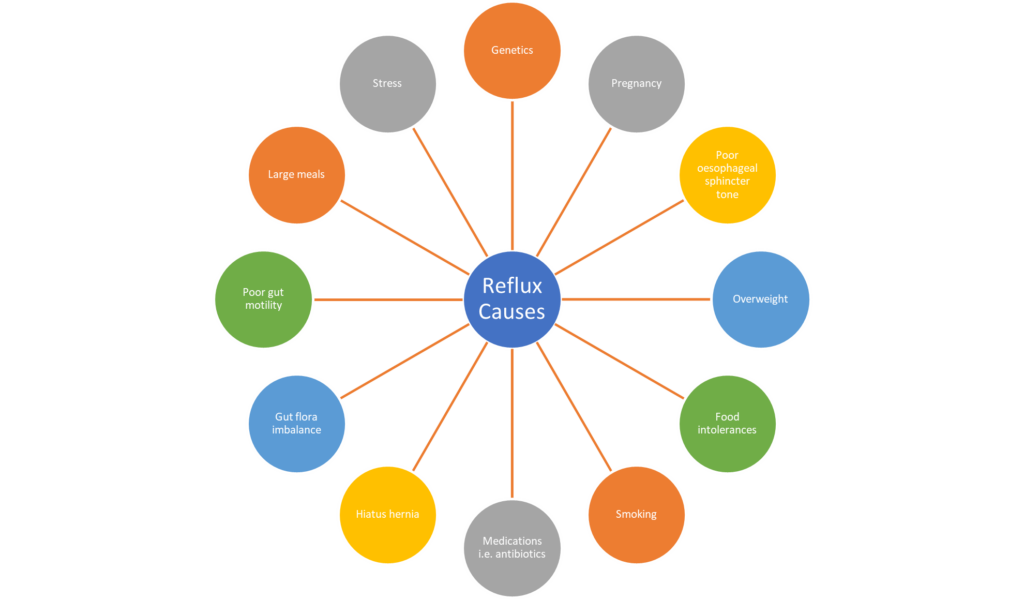
Reflux is multifactorial, and commonly caused by several factors in any one person. Naturopathically, my job is to isolate and uncover all contributing factors at play, and then use natural medicines to alleviate the symptoms and treat the causes. So, what are the possible contributing factors?
Poor oesophageal sphincter tone:
This is a feature of all cases of reflux. Poor tone of the sphincter allows stomach acid to escape and burn the lining of the oesophagus. For many this causes the sensation of burning experienced by most sufferers. My job is to uncover why you have lost the tone of this sphincter.
Fermentation of food by bacteria in the lower intestines causes the production of gasses. This gas causes backwards pressure on the stomach resulting in pressure on the sphincter, so it opens. Pressure can also be created by constipation and faecal impaction. Certain fermentable fibres can increase the risk of this, particularly fructooligosaccharides in foods like onion and garlic. If you are constipated or feel like you don’t empty your bowel properly, this will be one of the first considerations when formulating your treatment plan.
Genetics play a role in about 30% of reflux cases and can be a cause of lowered sphincter tone. It may be a case of hypermobility of muscle tissue such as that seed in Ehlers Danlos Syndrome or other underlying genetic factors.
Poor sleep is of upmost importance when looking at treating reflux. The sleep hormone melatonin is one of the few agents that have been researched to improve tone of the sphincter. If sleep evades you regularly, this will be a place to start with your treatment. Not only does melatonin improve the tone of the sphincter, but it is also a powerful antioxidant which aids the healing of the damaged tissue in the oesophagus.
Interestingly, another substance that has been studied and shown to improve the tone of the oesophageal sphincter, is psyllium husks. If you experience reflux, it may be worth giving this easy, home remedy a try before taking yourself to the doctor for reflux medications. Psyllium husks will not only improve tone of the sphincter but will also be a good source of dietary fibre, which may well treat the underlying cause if you are constipated or have an overgrowth of bad bacteria in the microbiome.
Health tip: Be sure to drink at least 3 litres of water each day when consuming psyllium husks as they absorb a lot of fluid in the gut and can lead to constipation if you are dehydrated.
There are substances which reduce sphincter tone that are best avoided. These include peppermint and peppermint oil products including peppermint tea, smoking, coffee, chocolate, and alcohol. Large meals and drinking fluids with meals, will overload the gut increasing the pressure in the stomach and on the sphincter. Similarly, eating too soon before laying down for bed will cause a delay in the emptying of the stomach leading to a backflow effect putting pressure on the sphincter.
Delayed gastric emptying and poor gut motility:
Consuming foods which are harder to digest or that slow down the emptying of your stomach, increase the pressure within the stomach and on the sphincter which causes acids to rise up the oesophagus. Foods high in fats, including chocolate, avocado and nuts, and alcohol slow down gastric emptying and increase reflux symptoms. Large meals also take longer to be digested and result in the same outcome.
Treatment for this include specific strains of probiotic (not all probiotics will help this issues) and the use of prokinetic agents, mainly herbs. There are a number of prokinetic herbs that can be used, such as chen pi or ginger. Switching your peppermint tea for ginger, may help improve reflux symptoms.
You may also have a condition which affects gastric motility, such as low serotonin in the gut or small intestinal bacterial overgrowth, or even adhesions from previous injury to the abdomen or surgeries (including appendectomy or caesarean births in some cases).
Endometriosis can also cause adhesions in some women affected. Agents that increase serotonin act as prokinetics, as serotonin in the gut improves gastric movement. Serotonin is the precursor to melatonin, and as mentioned previously, melatonin is one of the best remedies for improving sphincter tone and acting as an antioxidant to repair the damaged tissue in the oesophagus, therefore this intervention may have a multifaceted approach to the treatment of reflux.
The amino acid tryptophan can be useful for this, as well as a number of herbal medicines. Reducing stress too improves the gut brain axis, having a positive effect on reflux.
Decreased salivation:
This is another under considered cause of reflux. Salivation helps to move the gut along and alkalise the oesophagus, reducing the burning sensation. Some medications can cause dry mouth, particularly those used for colds and ADHD.
Chewing properly and the use of a good quality mastic gum chewing gum after meals can really improve reflux symptoms, reduce the burning, and improve gastric emptying. Not all chewing gum is appropriate as many brands contain toxic additives and plastics, which are hormone disruptors.
Bacterial imbalance in the small or large intestine:
An increase in bacteria in the small intestine leads to the fermentation of food and gas in the upper gut which can cause pressure on the stomach causing acid to rise up the oesophagus. A sign that this is a problem for you is that it likely started suddenly, possibly after a case of food poisoning or gastroenteritis and you now feel bloated and distended soon after meals. Even drinking water can cause bloating for some affected people.
Large intestinal dysbiosis usually results in bloating and distention towards the end of the day. Constipation can be a sign of either small or large bowel dysbiosis. The bad bacteria in the gut not only cause reflux and bloating, but they can contribute to many other health conditions and inflammatory symptoms.
Food intolerances:
Reflux can be a sign of food intolerance. The most common culprits are gluten and dairy. Try cutting these out of your diet along with high fat foods to see if your reflux improves. Interestingly, vegetarians experience reflux less often than omnivores. I advocate for a Mediterranean eating style which focuses on better quality sources of animal produce with an emphasis on consuming adequate fish.
Other factors to consider when treating reflux is abdominal obesity which increases fat around the stomach, pregnancy which causes reduced stomach volume to accommodate a foetus, smoking and hiatus hernia.
Naturopathic treatment:
Treatment includes addressing one or more of these underlying causes, removing dietary triggers, relieving the pain resulting from the burnt oesophagus with soothing herbs like aloe vera, reducing the damage to the tissue and healing the inflamed tissue with a high phytonutrient diet and antioxidant herbal medicines, improving the movement of the gut by addressing bacterial imbalances and encouraging gastric emptying with prokinetic agents, increasing salivation and improving sphincter tone.
Things to try before making an appointment with me:
- Chew foods thoroughly and consider purchasing a mastic gum chewing gum
- Avoid high fat meals
- Don’t eat too close to bed time
- Eat small meals and consider a Mediterranean diet
- Identify food triggers – the common ones are chocolate, alcohol, coffee, gluten and dairy.
- Quit smoking
- Try meditation to help stress levels and improve sleep quality
- Include psyllium husks in your diet
- Raise your bed head if you experience reflux when laying down
- Avoid carbonated drinks
- See a naturopath who holds a health gut practitioner certification by the Microbiome restoration centre
If you experience reflux, following a Mediterranean diet may help you in easing some of your symptoms. I have put together a guide to inform you about this common dietary approach which you can download here.
Share this Blog
If you enjoyed this article share it across your socials









